Actual lengths of stay at a hospital’s emergency department are a critical metric for assessing patient care efficiency and resource utilization. This article delves into the factors influencing variations in length of stay, industry benchmarks, and strategies for process optimization and intervention development to reduce actual lengths of stay.
Understanding the complexities of emergency department operations and implementing data-driven solutions are essential for improving patient outcomes and maximizing healthcare resources.
Actual Lengths of Stay at a Hospital’s Emergency Department
Actual lengths of stay (LOS) in emergency departments (EDs) vary widely. This variation can be attributed to a complex interplay of factors related to patients, providers, and the healthcare system itself. Understanding these factors and their impact is crucial for optimizing ED operations, improving patient outcomes, and ensuring efficient resource utilization.
Length of Stay Variations
Variations in LOS can be influenced by a range of factors, including:
- Patient-related factors:Age, comorbidities, severity of illness, social support, and patient preferences.
- Provider-related factors:Physician experience, staffing levels, and availability of specialists.
- System-related factors:ED overcrowding, availability of diagnostic and treatment resources, and discharge planning processes.
These factors can interact in complex ways, leading to significant variations in LOS. For example, an elderly patient with multiple comorbidities may have a longer LOS due to the need for more comprehensive evaluation and treatment. Similarly, an ED with limited staffing or diagnostic capabilities may experience longer LOS due to delays in patient care.
Variations in LOS can have important implications for patient outcomes and resource utilization. Prolonged LOS can lead to increased risk of complications, patient dissatisfaction, and higher healthcare costs. Conversely, shorter LOS can improve patient flow, reduce overcrowding, and free up resources for other patients.
Benchmarking and Comparison
Industry benchmarks for LOS in EDs provide a valuable reference point for evaluating the performance of individual hospitals. These benchmarks are typically established based on data from large cohorts of patients and can vary depending on factors such as the hospital’s location, patient population, and available resources.
By comparing actual LOS at a specific hospital to industry benchmarks, hospitals can identify areas for improvement and develop strategies to reduce LOS. For example, if a hospital’s LOS is significantly higher than the benchmark, it may indicate the need to address bottlenecks in the ED process or improve patient discharge planning.
Process Mapping and Optimization, Actual lengths of stay at a hospital’s emergency department
Process mapping is a valuable tool for identifying inefficiencies and bottlenecks that contribute to extended LOS. By creating a detailed map of the patient journey through the ED, hospitals can visualize the flow of patients and identify areas where delays or redundancies occur.
Once inefficiencies are identified, hospitals can propose and evaluate potential process improvements to reduce LOS. This may involve implementing new technologies, streamlining workflows, or enhancing communication between providers. For example, a hospital may implement an electronic health record system to improve access to patient information and reduce delays in ordering tests and medications.
Data Analysis and Visualization
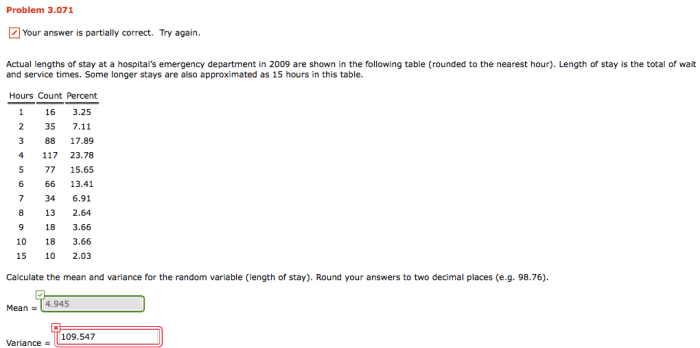
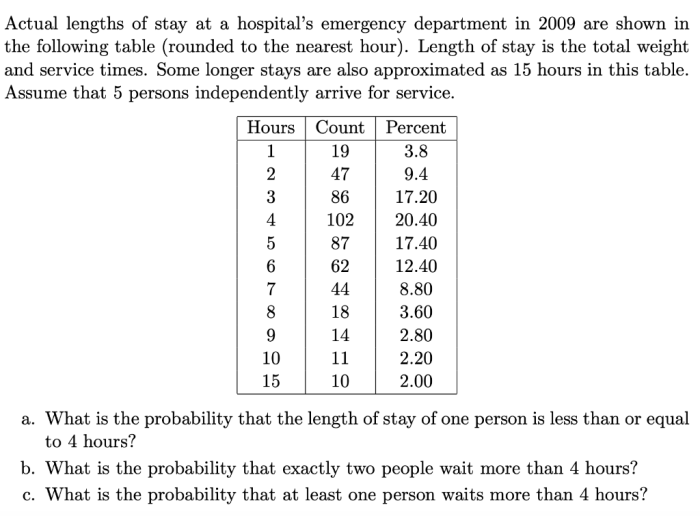
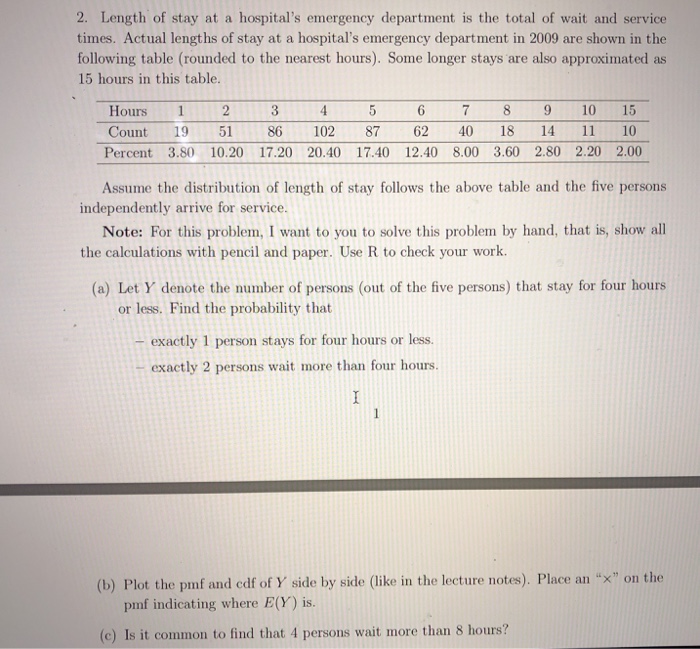
Data analysis and visualization are essential for understanding the patterns and trends in LOS. By collecting data on patient characteristics, provider practices, and system-related factors, hospitals can identify factors associated with longer LOS.
Visualizing the data using charts and graphs can help hospitals identify outliers, compare LOS across different patient populations, and track the effectiveness of process improvement initiatives. For example, a hospital may use a scatter plot to visualize the relationship between patient age and LOS, identifying the patient population that experiences the longest LOS.
Intervention Development and Implementation
Based on the insights gained from data analysis and process mapping, hospitals can develop and implement interventions aimed at reducing LOS. These interventions may include:
- Implementing fast-track protocols for low-acuity patients.
- Enhancing communication between providers to reduce delays in patient care.
- Providing dedicated discharge planning services to expedite patient discharge.
- Improving patient education and self-management skills to reduce the need for repeat visits.
The effectiveness of these interventions should be monitored and evaluated using appropriate metrics, such as average LOS, patient satisfaction, and resource utilization. By continuously monitoring and refining their interventions, hospitals can optimize ED operations and improve patient outcomes.
Top FAQs
What are the primary factors that influence variations in actual lengths of stay in the emergency department?
Patient-related factors (e.g., age, acuity), provider-related factors (e.g., staffing levels, triage practices), and system-related factors (e.g., bed availability, hospital policies) all contribute to variations in length of stay.
How are industry benchmarks for actual lengths of stay established?
Industry benchmarks are typically derived from national databases or multi-center studies that collect data on patient demographics, triage categories, and length of stay outcomes.
What are some potential interventions to reduce actual lengths of stay in the emergency department?
Interventions may include implementing fast-track protocols, improving triage accuracy, enhancing patient communication, and optimizing staffing levels to match patient demand.